From Flea Bites to Fierce Advocacy: How a Rare Disease Nearly Took Me Down—And What It Taught Me
I thought I was just run-down. I ended up in the ICU with a disease I’d never heard of.
Note: This is a story about trusting your gut. About advocating for yourself when no one else seems to be listening. It’s about illness, fear, and the very real cracks in our healthcare system. But mostly, it’s a story about resilience, motherhood, and the community that carried me when I couldn’t carry myself.
Let’s rewind to last spring (2024).
(Above: Easter 2024…later that night I started aching in my legs)
Easter had just wrapped. My parents were heading back to Ohio after visiting for several days, and life was supposed to return to normal. Instead, I started noticing a weird ache in my legs. Nothing dramatic—just that kind of low-grade pain that makes you feel off. At night, I got minor chills. I took Tylenol and shrugged it off. I’m a mom of three. Feeling rundown is just part of the job.
By Wednesday, the aches were worse, and now I had a fever. 102 and climbing. I told myself it was just a lingering virus and my body was trying to fight it. I canceled a few things. Rested. Pushed fluids. Tried to carry on. As moms do, right?
But by the weekend, my body gave up. I could barely move. I wasn’t sleeping. I couldn’t parent. I couldn’t even sit up for long. I lived on smoothies and broth. And the headache kicked in. WOW. The headache. The worst of my life.
My husband moved to the pull-out couch while I turned our bedroom into a cave of sweat-soaked sheets and silent worry. Something was clearly wrong. But I still didn’t know just how bad it was going to get. And no one in the house except me felt any of these symptoms…I knew something was up.
After five or six days of fever, aches, and complete exhaustion, we went to a walk-in ER. I underwent a full workup—flu, COVID, strep. All negative. Just to be safe, they tested me for meningitis with a spinal tap. That alone was one of the most physically traumatic things I’ve ever experienced. But I wanted answers and was willing to do anything. They sent me home with a round of steroids and antibiotics, told me to rest, and said it was probably viral.
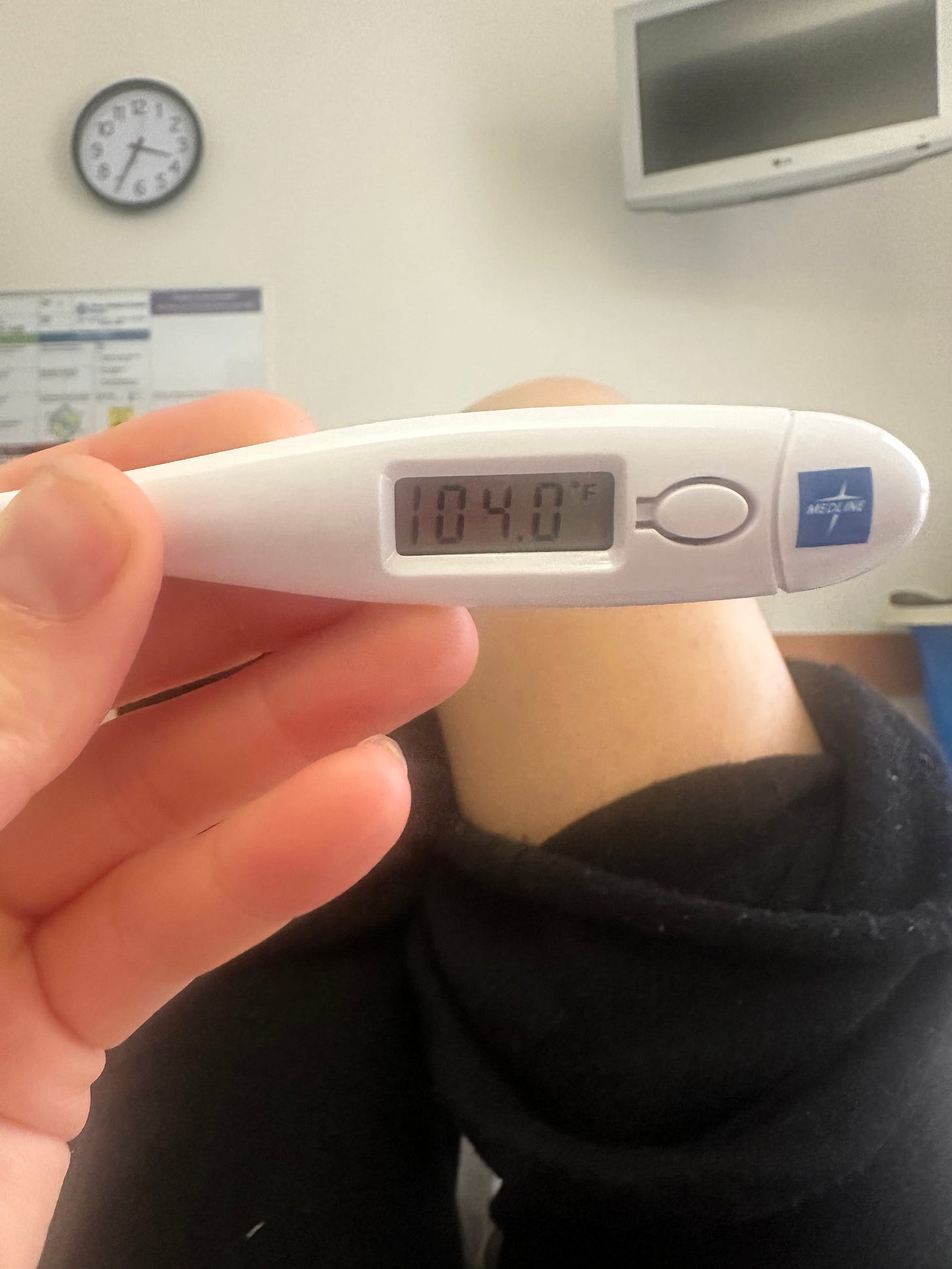
I tried. But just hours later, my fever returned with a vengeance. 104. It spiked so fast it scared me. That’s when I woke Bill up in the middle of the night and we drove to the bigger hospital.
(Above: my fever was hovering around 103/104 for days)
I walked—or rather, stumbled—into the ER with the hope of finally getting answers. But instead of help, I was met with doubt. They looked at my charts from just 12 hours earlier and echoed that whatever I had was probably “just viral.” I could feel them writing me off. I could see it in the Resident’s body language: she was pegging me as just another tired mom, probably anxious, probably overreacting.
(Above: this is me in ER, waiting for answers)
But I knew. My body was screaming at me that this wasn’t normal. So I did something I’ve learned to do, even when it feels uncomfortable: I advocated for myself.
Eventually, I was admitted for further observation. As this journey unfolded I would pop on Instagram to give my followers an update. Despite feeling miserable, posting was a Hail Mary because I was hoping maybe someone in my community would have answers. Sure enough, one of my followers pushed me to ask to see an infectious disease doctor. Something neither Bill or I had thought of yet. So late into the evening I asked to see an infectious disease specialist. That decision may have saved my life.
He reviewed my symptoms and started asking questions that made me stop in my tracks. Had I been around any animals? Stray cats? Opossums? Had my kids been playing in tall grass or on sports fields recently?
NO? I mean, maybe? We live in a city - I mean downtown Austin is a mere two miles away. But have I seen possums and raccoons in my own backyard? Yes. Am I out on soccer fields nearly every weekend with my kids? Yes. Had I remembered a flea bite? Absolutely not.
He suspected murine typhus, a rare and serious bacterial infection spread by fleas—especially here in Texas. He said he sees about 8-10 cases per year in Austin and mine fit the profile. He also shared that this disease is really only prevalent in Texas, California and Hawaii, but that Austin had such a high case in the early 2000s that the CDC had come here to study the disease in more depth. He said said most people never even notice when they are bitten by a flea. The bite is usually microscopic. And it likely happened 10-14 days ago and so it likely wasn’t even on my radar. My severe migraine and high fever were two very strong signs that this was what I had. The blood test would take two-three weeks to get results, so he wanted to treat me right away regardless of my confirmed diagnosis.
There was just one problem: the standard treatment is doxycycline, and I’m allergic to it. So they started me on a high-dose azithromycin protocol instead.
That night, everything changed. And not in a good way.
I began to shake uncontrollably. My blood pressure dropped dangerously low. I was rushed to the ICU. My veins had collapsed from dehydration and repeated IV attempts, so they inserted a PICC line. I was in full-blown sepsis. Things got very serious, very quickly.
(Above: a video I recorded the day after I went septic. I was a mess and very emotional.)
The days that followed were a haze of pain and fear—crippling migraines, round-the-clock vitals, and a flurry of concerned faces. I remember watching the concern on the nurses’ faces and realizing for the first time: this is not just a bad week. This is life-threatening. The doctor kept reassuring me things could get worse before they got better. That the antibiotics might take longer to work because it was a second line treatment. I just didn’t expect it to get THIS bad.
I was on a strong cocktail of morphine, dilaudid and other strong pain meds for days….drugs I’d only ever heard of for Cancer patients. As soon as one wore off I was given another. The headache felt like a hammer to my head. A constant “1, 2, 3” beat that never ceased.
My mom flew back from Ohio to be by my side. My husband balanced the impossible: caring for three kids, trying to work, and visiting me daily with updates and back rubs. Friends dropped off meals and migraine packs for my head. Neighbors helped juggle pickups and drop-offs. A girlfriend came in just to blow dry my hair. My friends and their daughters staged an entire photoshoot on my behalf for my new pajama line. Those same girlfriends - and one of their moms AND my mom- set up a table scape on my behalf at a charity event I had committed to. My nanny fulfilled quilted jacket orders for me (an item that just happened to arrive from India while I was in the hospital). Everyone rallied. It still makes me emotional to think about how held we were during that time.
(Above: one of my girlfriends - Kim - who came to the hospital to check on my and blow dry my hair)
And then—because I’m a chronic oversharer and I believe in the power of connection—I continued to share my story on Instagram.
The messages started pouring in. People who had never heard of murine typhus. People who lived in Texas and recognized similar symptoms in themselves or their kids. One woman in Dallas who had just recovered from it two weeks prior. Another who’s son almost died from it. People praying for me, checking on me. Loving me from afar whether they knew me or not.
(Above: some of the messages - I got hundreds - I received on Instagram while I was in the hospital.)
After nearly ten long days, I was discharged from the hospital. I was wheeled out of the hospital a changed woman. The contrast of the white, drab walls of the hospital with the bright Texas sun in the parking lot was stark. I hadn’t seen sunlight in days. I had lost over 10 lbs in 10 days as I had almost zero appetite and barely moved from my bed until my final day in the hospital.
(Above: a screenshot of me leaving the hospital after 10 long days)
Yes, I was recovering physically. But emotionally? I was unraveling. The adrenaline that had carried me collapsed. I cried constantly that first week. I questioned everything—how long I had ignored my own symptoms, how hard I had to push just to be believed, how close I came to a very different outcome and how horrible that would have been for my children (who we had kept shielded from most of this during my stay).
After the first few weeks of settling I realized this wasn’t just my story—it was one that could actually help people.
A year later, I still get messages about Murine Typhus. I saved all of my IG stories in a highlight reel and I still field DMs from people asking about symptoms, doctors, what to say to get taken seriously. And I always write back. Because if this happened to me—someone with access, education, support—it can happen to anyone.
This story could’ve ended very differently. But it didn’t.
And that, I’ve learned, is reason enough to tell it.
I want to be clear: I know I’m not a cancer patient. I wasn’t away from my children for months. What I went through is not the same as the long, harrowing medical journeys many families face every day. But it was traumatic for me and our family. It was a full stop—a reminder that our health is fragile, and our systems are flawed. It shook me. And for a few terrifying days, I truly didn’t know how—or if—I’d come out the other side.
(Above: a couple of the messages I’ve from people who found my Instagram account and have gotten treatment for Murine Typhus because of my stories).
Telling this story is my way of honoring that experience—and hopefully, helping someone else find their voice a little sooner than I did. Or helping people whose lives were potentially saved because I shared so openly. I don’t say any of that to brag…but because it finally felt like my trauma had a purpose.
This story could’ve ended very differently. But it didn’t.
And that, I’ve learned, is reason enough to tell it.
Here’s what I know for sure:
1. Trust your gut. If something feels off, speak up. Push harder. You know your body better than anyone.
2. Find your people. Whether it’s a partner, a parent, a neighbor or a best friend who flies across the country—let them help. We are not meant to carry everything alone.
3. Tell the story. We live in a culture that’s quick to dismiss, especially women and especially mothers. When we share what we’ve been through, we chip away at that. We make space for someone else to speak up too.
✅ Murine Typhus Symptom Checklist
NOTE: THIS IS NOT MEDICAL ADVICE. PLEASE CONSULT YOUR DOCTOR OR NEAREST ER. That said, if you’ve been feeling “off” and live in an area where murine typhus is present (especially Texas, California, or Hawaii), here are the symptoms to watch for (and that I personally experienced)
High fever (often 102°F or higher) that doesn’t go away
Severe fatigue or body aches that feel worse than a typical flu
Chills or shaking episodes
Headache, often intense or persistent
Muscle pain or joint pain, especially in the legs or lower back
Nausea or vomiting
Loss of appetite
Cough (in some cases) - mine came about 10 days in
Rash (may appear around day 5–6, though not always - but mine came about a week in)
Confusion or lightheadedness (a possible sign of sepsis)
💡 When to seek medical care:
If you’ve had these symptoms for several days, especially after outdoor exposure or contact with animals (stray cats, opossums, rodents), and you’ve ruled out flu, COVID, and strep—ask to see an infectious disease doctor to test for murine typhus. It’s rare but on the rise in some states.
🩺 Treatment: Doxycycline is the first-line treatment, but there are alternatives if you’re allergic like me—be sure to tell your doctor.